Leonie Wheeldon, a Consultant Biomedical Scientist specialising in cytopathology, discusses her work on rapid onsite evaluation.
At a glance
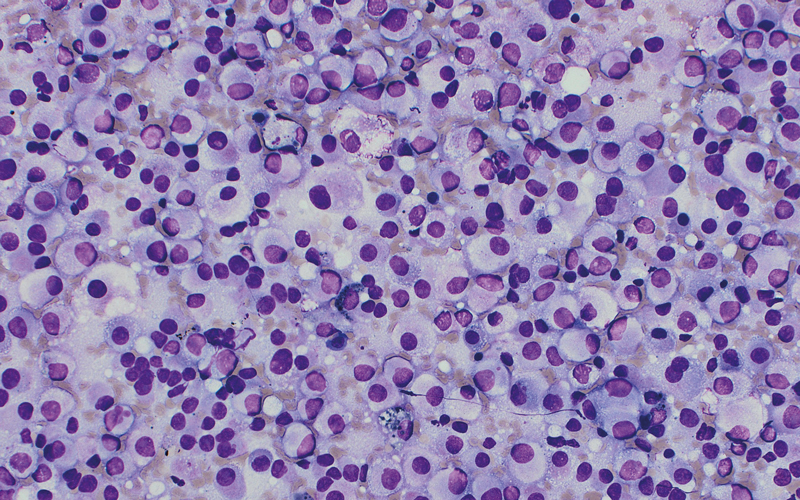
- ROSE provides a real-time morphological assessment of cytology specimens during medical procedures.
- It helps to ensure that sufficient diagnostic material is obtained and samples are triaged and sent to microbiology, flow cytometry and biochemistry. A biopsy can even be obtained in the same appointment.
- ROSE should optimise the procedure and inform patient management, streamlining the diagnostic pathway.
Described by Advancing Healthcare Awards (AHAwards) judges as “energetic and inspiring”, Leonie Wheeldon, who has been named Biomedical Scientist of the Year, says she “fell” into cytology while interviewing for a trainee biomedical scientist post after getting her BSc in 2005.
But she adds: “In no time at all my passion for cytology was ignited and I really felt this was the career for me. Motivation to do more, learn more, develop more and provide the best service for patients came naturally, simply because I enjoyed doing it, and it’s never faded to this day.”
Leonie says she was led to her work on the practice of rapid onsite evaluation (ROSE) – in which material acquired at fine needle aspiration (FNA) of suspicious masses in patients is assessed in clinic to confirm that the right amount of the right material has been acquired, reducing the need for repeat sampling – by “the right place and right time, and the love of cells”.
“As a Trainee Biomedical Scientist I regularly attended bronchoscopy, breast and head and neck clinics to help make high-quality slide preparations and needle core imprints,” she says.
“I could clearly see the positive impact that cytology presence had at ensuring the samples were high quality and triaged appropriately, leading to accurate and timely results, ultimately improving patient care.”
Multidisciplinary working
It was while working as Senior Biomedical Scientist training endoscopy nurses on how to best prepare bronchial and common bile duct brushings for liquid-based cytology, Leonie got talking to a respiratory consultant and a radiologist.
“They were discussing how they could implement an endobronchial ultrasound (EBUS) service for the diagnosis and staging of lung cancer and an endoscopic ultrasound (EUS) service for pancreatic lesions,” she says. “They were very keen to have immediate cytology feedback on the quality and adequacy of the cytology samples particularly as they were learning themselves. This very much aligned with my focus on innovative practice and development of diagnostic cytology services.”
News spread amongst the clinicians in the trust about the value of working closely with cytology colleagues, and ROSE – which involves collaborative multidisciplinary team working and providing real-time morphological assessment of cytology specimens during medical procedures – has continued to grow ever since.
The service currently offers eight clinics a week served by a team of biomedical scientists and pathologists covering EBUS, EUS (pancreas, mediastinal, gastrointestinal, left adrenal and liver lesions) and head and neck, benefiting approximately 500 patients every year.
Effective triaging
ROSE helps to ensure that sufficient diagnostic material is obtained and samples are triaged and sent to microbiology, flow cytometry and biochemistry. A biopsy can even be obtained in the same appointment. This prevents the patient from having to return to the hospital for repeat or more invasive procedures.
ROSE improves patient outcomes in a number of ways. “Medical advances have resulted in smaller needles to minimise risk of complications to patients. The requirements from these smaller samples in terms of tumour profiling and molecular testing is constantly growing as more personalised therapies become available,” Leonie says.
The practice can reduce the procedure time by decreasing the number of times the needle has to pass into the area of interest.
ROSE also enables immediate feedback of sample viability during the procedure, prompting the clinician to sample alternative sites to obtain optimal-quality samples. The rapid evaluation of cytology specimens allows for quicker initiation of appropriate treatment plans, and it facilitates real-time communication between healthcare professionals.
Wider adoption
ROSE is resource-intensive, requiring trained and competency-assessed personnel, with quality assurance to mitigate risks of false-negative results from ceasing the procedure too soon, or false-positive results from unnecessarily prolonging a procedure.
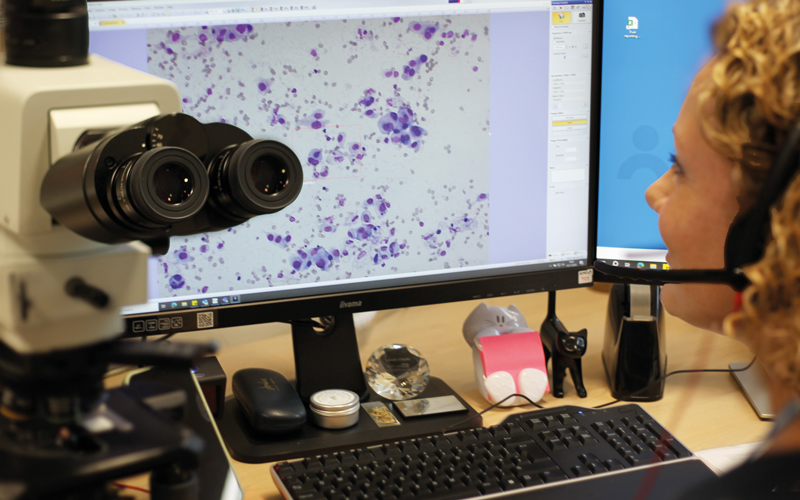
Leonie’s trust – Royal Cornwall Hospitals NHS – has implemented telecytology ROSE for community sites away from the cytology lab to reduce the resource burden and continue to increase accessibility for patients in the head and neck cancer pathway. “We use a clinical imaging assistant to prepare samples and operate the microscope, which eliminates travel and wait time between procedures, resulting in minimal burden on cytology resources,” Leonie says.
The British Association for Cytopathology – Leonie is a member of its Executive – is working with multiple bodies to encourage widespread adoption of best practice and improve the number of cytology departments that provide ROSE in the UK. Collaborative working with a range of colleges, institutions and associations has raised awareness of the benefits of ROSE and led to the creation of evidence-based documented guidance.
Leonie has been involved in piloting a new ROSE qualification for IBMS members to facilitate wider adoption nationally. “This year saw the first three-day training course dedicated to ROSE,” says Leonie, who is IBMS Cytopathology Specialist Advisory Panel Deputy Chair. “As the value of ROSE continues to grow in diagnostic and therapeutic procedures, we hope to see an increasing number of biomedical scientists pursuing training and qualifications in this area to meet evolving clinical demands and contribute to improved patient care pathways,” she says.
Improving patient experience and outcome is a major motivator for Leonie, and it’s not surprising the AHAwards judges also said her “powerful combination of service innovation and biomedical scientist training” has international reach and she is an ambassador for the profession. “I’m so proud of the cytology and histology teams here. We have such good relationships with the clinical teams and this collaborative approach alongside the staff dedication is really making a difference to people’s lives in our local community,” she concludes.
Explore further
- Leonie’s paper in Cytopathology: bit.ly/4dRrcuX
- Information on ROSE single slide assessment: bit.ly/3Vb1ESo
- IBMS’ Specialist diploma: ROSE module: bit.ly/4dRPrcA
Image credit | Leonie Wheeldon